Tuberculosis (commonly shortened to TB) is an infection caused by the bacterium Mycobacterium tuberculosis, which most commonly affects the lungs (pulmonary TB) but can also affect the central nervous system (meningitis), lymphatic system, circulatory system (Miliary tuberculosis), genitourinary system, bones and joints.
Tuberculosis is one of the most deadly and common major infectious diseases today, infecting two billion people, or approximately one-third ( WHO TB.) of the world's population. Nine million new cases of disease, resulting in two million deaths, occur annually, mostly in developing countries. However, developed countries are not spared the burden of tuberculosis. There is a rising proportion of people who are immunocompromised, either due to immunosupressive drugs or HIV/AIDS. These people are at particular risk of tuberculosis infection and active tuberculosis disease.
Most of those infected (90%) have asymptomatic latent TB infection (LTBI). There is a 10% lifetime chance that LTBI will progress to TB disease which, if left untreated, will kill more than 50% of its victims. TB is one of the top three infectious killing diseases in the world: HIV/AIDS kills 3 million people each year, TB kills 2 million, and malaria kills 1 million.
The neglect of TB control programs, HIV/AIDS, and immigration has caused a resurgence of tuberculosis. Multiple drug resistant strains of TB (MDR-TB) and Extreme Drug-Resistance in Tuberculosis (XDR-TB) are emerging. The World Health Organization declared TB a global health emergency in 1993, and the Stop TB Partnership proposed a Global Plan to Stop Tuberculosis which aims to save an additional 14 million lives between 2006 and 2015.
Other names for the disease
TB (short for tuberculosis and also for Tubercle Bacillus)
Consumption (TB seemed to consume people from within with its symptoms of bloody cough, fever, pallor, and long relentless wasting)
Wasting disease
White plague (TB sufferers appear markedly pale)
Phthisis (Greek for consumption) and phthisis pulmonalis
Scrofula (swollen neck glands)
King's evil (so called because it was believed that a king's touch would heal scrofula)
Pott's disease of the spine
Miliary TB (x-ray lesions look like millet seeds)
Tabes mesenterica (TB of the abdomen)
Lupus vulgaris (the common wolf - TB of the skin)
Prosector's wart, also a kind of TB of the skin, transmitted by contact with contaminated cadavers to anatomists, pathologists, veterinarians, surgeons, butchers, etc.
Koch's Disease named after Robert Koch who discovered the tuberculosis bacilli.
The bacterium
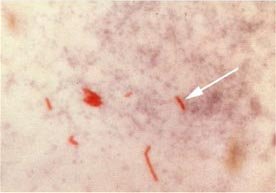
Acid-fast bacilli (AFB) (shown in red) are tubercle bacilli Mycobacterium tuberculosis.
The cause of tuberculosis, Mycobacterium tuberculosis (MTB), is a slow-growing aerobic bacterium that divides every 16 to 20 hours. This is extremely slow compared to other bacteria (although not the slowest), which tend to have division times measured in minutes (among the fastest growing bacteria is a strain of E. coli that can divide roughly every 20 minutes; by contrast, Mycobacterium leprae divides every 20 days). MTB is not classified as either Gram-positive or Gram-negative because it does not have the chemical characteristics of either, although it contains peptidoglycan in the cell wall, which means it is related to the Gram-positive organisms. If a Gram stain is performed, it stains very weakly Gram-positive or not at all (ghost cells). It is a small rod-like bacillus which can withstand weak disinfectants and can survive in a dry state for weeks but, spontaneously, can only grow within a host organism (in vitro culture of M. tuberculosis took a long time to be achieved, but is nowadays a routine laboratory procedure).
MTB is identified microscopically by its staining characteristics: it retains certain stains after being treated with acidic solution, and is thus classified as an "acid-fast bacillus" or "AFB". In the most common staining technique, the Ziehl-Neelsen stain, AFB are stained a bright red which stands out clearly against a blue background. Acid-fast bacilli can also be visualized by fluorescent microscopy, and by an auramine-rhodamine stain.
The M. tuberculosis complex includes 3 other mycobacteria which can cause tuberculosis: M. bovis, M. africanum, and M. microti. The first two are very rare causes of disease and the last one does not cause human disease.
Nontuberculous mycobacteria (NTM) are other mycobacteria (besides M. leprae which causes leprosy) which may cause pulmonary disease resembling TB, lymphadenitis, skin disease, or disseminated disease. These include Mycobacterium avium, M. kansasii, and others.
The disease Transmission
TB is spread by aerosol droplets expelled by people with active TB disease of the lungs when they cough, sneeze, speak, or spit. Each droplet is 5 µm in diameter and contains 1 to 3 bacilli. Close contacts (people with prolonged, frequent, or intense contact) are at highest risk of becoming infected (typically a 22% infection rate). A person with untreated, active tuberculosis can infect an estimated 20 other people per year. Others at risk include foreign-born from areas where TB is common, immunocompromised patients (eg. HIV/AIDS), residents and employees of high-risk congregate settings, health care workers who serve high-risk clients, medically underserved, low-income populations, high-risk racial or ethnic minority populations, children exposed to adults in high-risk categories, and people who inject illicit drugs.
Transmission can only occur from people with active TB disease (not latent TB infection).
The probability of transmission depends upon infectiousness of the person with TB (quantity expelled), environment of exposure, duration of exposure, and virulence of the organism.
The chain of transmission can be stopped by isolating patients with active disease and starting effective anti-tuberculous therapy.
Pathogenesis
While only 10% of TB infection progresses to TB disease, if untreated the death rate is 51%.
TB infection begins when MTB bacilli reach the pulmonary alveoli, infecting alveolar macrophages, where the mycobacteria replicate exponentially. The primary site of infection in the lungs is called the Ghon focus. Bacteria are picked up by dendritic cells, which can transport the bacilli to local (mediastinal) lymph nodes, and then through the bloodstream to the more distant tissues and organs where TB disease could potentially develop: lung apices, peripheral lymph nodes, kidneys, brain, and bone.
Tuberculosis is classed as one of the granulomatous inflammatory conditions. Macrophages, T lymphocytes, B lymphocytes and fibroblasts are among the cells that aggregate to form a granuloma, with lymphocytes surrounding infected macrophages. The granuloma functions not only to prevent dissemination of the mycobacteria, but also provides a local environment for communication of cells of the immune system. Within the granuloma, T lymphocytes (CD4+) secrete a cytokine such as interferon gamma, which activates macrophages to destroy the bacteria with which they are infected, making them better able to fight infection. T lymphocytes (CD8+) can also directly kill infected cells.
Importantly, bacteria are not eliminated with the granuloma, but can become dormant, resulting in a latent infection. Latent infection can be diagnosed only by tuberculin skin test, which yields a delayed hypertype sensitivity response to purified protein derivatives of M. tuberculosis in an infected person.
Another feature of the granulomas of human tuberculosis is the development of cell death, also called necrosis, in the center of tubercles. To the naked eye this has the texture of soft white cheese and was termed caseous necrosis.
If TB bacteria gain entry to the blood stream from an area of tissue damage they spread through the body and set up myriad foci of infection, all appearing as tiny white tubercles in the tissues. This is called miliary tuberculosis and has a high case fatality.
In many patients the infection waxes and wanes. Tissue destruction and necrosis are balanced by healing and fibrosis. Affected tissue is replaced by scarring and cavities filled with cheese-like white necrotic material. During active disease, some of these cavities are in continuity with the air passages bronchi. This material may therefore be coughed up. It contains living bacteria and can pass on infection.
Treatment with appropriate antibiotics kills bacteria and allows healing to take place. Affected areas are eventually replaced by scar tissue.
Progression
In those people in whom TB bacilli overcome the immune system defenses and begin to multiply, there is progression from TB infection to TB disease. This may occur soon after infection (primary TB disease – 1 to 5%) or many years after infection (post primary TB, secondary TB, reactivation TB disease of dormant bacilli – 5 to 9%). The risk of reactivation increases with immune compromise, such as that caused by infection with HIV. In patients co-infected with M. tuberculosis and HIV, the risk of reactivation increases to 10% per year, while in immune competent individuals, the risk is between 5 and 10% in a lifetime.
About five percent of infected persons will develop TB disease in the first two years, and another five percent will develop disease later in life. In all, about 10% of infected persons with normal immune systems will develop TB disease in their lifetime.
Some medical conditions increase the risk of progression to TB disease. In HIV infected persons with TB infection, the risk increases to 10% each year instead of 10% over a lifetime. Other such conditions include drug injection (mainly because of the life style of IV Drug users), substance abuse, recent TB infection (within two years) or history of inadequately treated TB, chest X-ray suggestive of previous TB (fibrotic lesions and nodules), diabetes mellitus, silicosis, prolonged corticosteroid therapy and other immunosuppressive therapy, head and neck cancers, hematologic and reticuloendothelial diseases (leukemia and Hodgkin's disease), end-stage renal disease, intestinal bypass or gastrectomy, chronic malabsorption syndromes, or low body weight (10% or more below the ideal).
Some drugs, including rheumatoid arthritis drugs that work by blocking tumor necrosis factor-alpha (an inflammation-causing cytokine), raise the risk of causing a latent infection to become active due to the importance of this cytokine in the immune defense against TB.
TB disease most commonly affects the lungs (75% or more), where it is called pulmonary TB. Symptoms include a productive, prolonged cough of more than three weeks duration, chest pain, and hemoptysis. Systemic symptoms include fever, chills, night sweats, appetite loss, weight loss, and easy fatigability. The term consumption arose because sufferers appeared as if they were "consumed" from within by the disease. People from Asian and African descent may have more often lymph node TB than Caucasians.
Extrapulmonary sites include the pleura, central nervous system (meningitis), lymphatic system (scrofula of the neck), genitourinary system, and bones and joints (Pott's disease of the spine). An especially serious form is "disseminated", or "miliary" TB, so named because the lung lesions so-formed resemble millet seeds on x-ray. These are more common in immunosuppressed persons and in young children. Pulmonary TB may co-exist with extrapulmonary TB.
Drug resistance
Drug-resistant TB is transmitted in the same way as regular TB. Primary resistance develops in persons initially infected with resistant organisms. Secondary resistance (acquired resistance) may develop during TB therapy due to inadequate treatment regimen, not taking the prescribed regimen appropriately or using low quality medication.
Diagnosis
A complete medical evaluation for TB includes a medical history, a physical examination, a tuberculin skin test, a serological test, a chest X-ray, and microbiologic smears and cultures. The measurement of a positive skin test depends upon the person's risk factors for progression of TB infection to TB disease. Bacteriophage-based assays are among a few new testing procedures that offer the hope of cheap, fast and accurate TB testing for the impoverished countries that need it most.
See: tuberculosis diagnosis, tuberculosis radiology
Treatment
Persons with TB infection (class 2 or class 4 TB), but who do not have TB disease (class 3 or class 5 TB), cannot spread the infection to other people. TB infection in a person who does not have TB disease is not considered a case of TB and is often referred to as latent TB infection (LTBI). This distinction is important because treatment options will be different for a person who has LTBI instead of active TB disease.
See: tuberculosis treatment
Prevention of Tuberculosis
Prevention and control efforts include three priority strategies:
identifying and treating all persons who have TB disease
finding and evaluating persons who have been in contact with TB patients to determine whether they have TB infection or disease, and treating them appropriately, and
testing high-risk groups for TB infection to identify candidates for treatment of latent infection and to ensure the completion of treatment.
In tropical areas where the incidence of atypical mycobacteria is high, exposure to nontuberculous mycobacteria gives some protection against TB.
BCG vaccine
Many countries use BCG vaccine as part of their TB control programs, especially for infants. The protective efficacy of BCG for preventing serious forms of TB (e.g. meningitis) in children is high (greater than 80%). However, the protective efficacy for preventing pulmonary TB in adolescents and adults is variable, from 0 to 80%. In the United Kingdom, children aged 10-14 were typically immunized during school until 2005. (Routine BCG vaccination was stopped as it was no longer cost-effective. The incidence of TB in people born in the UK, and with parents and grandparents who were born in the UK, was at an all time low, and falling. Others continue to be offered BCG vaccination.)
The effectiveness of BCG is much lower in areas where mycobacteria are less prevalent. In the USA, BCG vaccine is not routinely recommended except for selected persons who meet specific criteria:
Infants or children with negative skin-test result who are continually exposed to untreated or ineffectively treated patients or will be continually exposed to multi-drug resistant TB.
Healthcare workers considered on individual basis in settings in which high percentage of MDR-TB patients has been found, transmission of MDR-TB is likely, and TB control precautions have been implemented and not successful.
Tuberculosis vaccine
The first recombinant tuberculosis vaccine entered clinical trials in the United States in 2004 sponsored by the National Institute of Allergy and Infectious Diseases (NIAID). [1]
A 2005 study showed that a DNA TB vaccine given with conventional chemotherapy can accelerate the disappearance of bacteria as well as protecting against re-infection in mice; it may take four to five years to be available in humans. PMID 15690060.
Because of the limitations of current vaccines, researchers and policymakers are promoting new economic models of vaccine development including prizes, tax incentives and advance market commitments